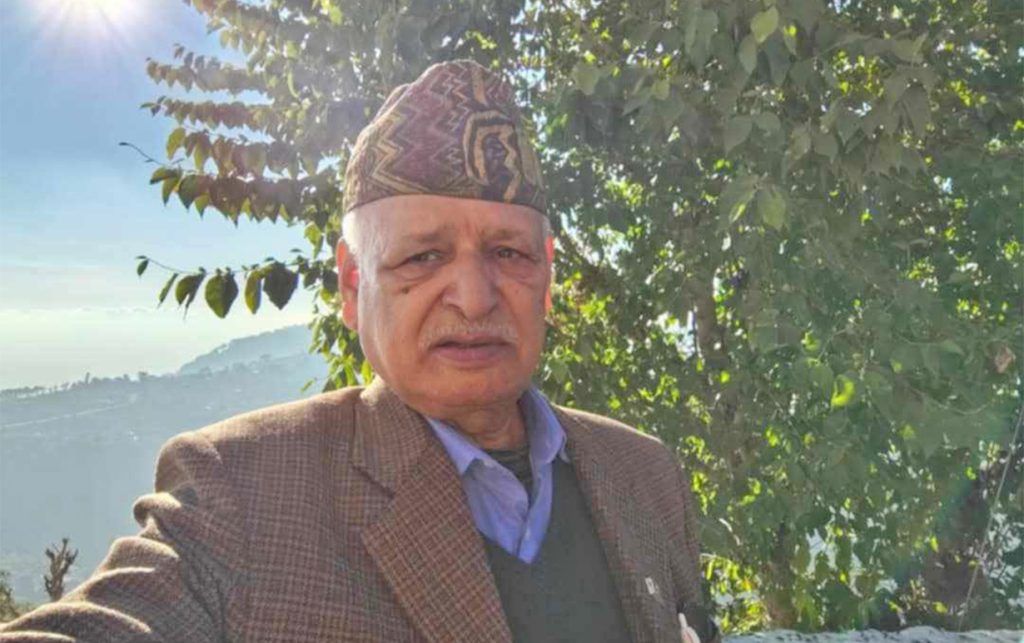
Dr Ramu Kharel, from Nepal, is currently based in Georgia, the US. He is busy taking care of the patients infected with coronavirus at a local hospital’s emergency ward. OnlineKhabar recently talked with Kharel about his experience of being in the front line of treating coronavirus patients, security measures required for the health workers during this time and what Nepal learn from the experiences of people like him.
Excerpts:
What are the stages a patient infected with coronavirus has to go through for treatment?
When a patient comes to our emergency department, we first measure their temperatures, then look at other symptoms followed by a series of questions. If they show relatable symptoms, they are called “persons under investigations” and we give them a surgical mask. Based on their symptoms, we categorise the patients into different categories with high, medium and minimum risks. They are kept in separate rooms and we take a nasopharyngeal swab [from their nose].
People who do not have respiratory problems and who do not have chronic diseases are sent home for quarantine and prescribed medicine against fever. Once the test results are out, we inform those patients. If the patients have to be admitted to the hospital, we treat them according to their respiratory conditions.
Across the world, thousands have died after contracting the virus. Why do you think the death toll is so high this time?
The case fatality rate of Covid-19 is 2-4 per cent anywhere. There are different factors behind this. The first is that the virus affects the respiratory system worse than other viruses, resulting in acute respiratory distress syndrome and then death. Furthermore, it affects people with other chronic illnesses more just like other viruses and the death toll increases. Another reason is that it is easily transmitted and it is estimated that 40 to 60 percent of the world population will be infected by the virus. There is a chance that our health system will be overwhelmed by it, resulting in more deaths.
What are the differences between the treatment of Covid-19 patients and other patients?
The problem with the coronavirus is that even the healthiest-looking person can be a carrier of the virus while it heavily affects those with other chronic illnesses. It does not have any definite cure yet, and its vaccine will likely take some 18 months before we get one as per infectious disease experts. As we are still in the process of understanding the virus; new information and new protocols are coming out every day. So, it is crucial that doctors follow the security protocols on the dot as well as stay updated with the newest developments, and treat patients accordingly.
Were you involved in treatment against coronavirus-like viruses before this?
There were many other viruses similar to this coronavirus in the past, and they all cause similar symptoms like cold, cough, and fever. However, the attack on the lungs as seen in the Covid-19 patients is worse and that results in death in severe conditions. But a majority of the patients have recovered and are symptomatically treated.
Being at the frontline, how do you see the mental state of the patients in the hospital?
The emergency ward in my hospital is one of the busiest in the US. About 6,000 cases of coronavirus have been reported in the state (Georgia) so far, and among them, 100 are being treated in the hospital right now. Definitely, the fear of the virus has gripped people here as well. The patients are scared and there is a lot of mental stress among them. And this is true even among those who have mild symptoms.
On the other hand, how is the mental state of the doctors who are constantly treating the patients?
The doctors are also facing a high level of stress right now, with so many deaths and social turmoil around us. Doctors from cities like New York where there is a higher number of cases face a higher level of risk. They do not have personal protective equipment (PPE), or ventilators for critical patients in the hospitals. As a result, many have died. The stress in this situation is expected.
Many of my colleagues have children and also other elderly people at home. In such conditions, extra stress is added as they have to get isolated from their own family members.
What are the precautionary measures the doctors working at the frontline need to follow?
While treating the patients, those infected with and suspected of coronavirus infection both, the doctors have to follow the “universal assumption of risk”, a defensive approach, to avoid contracting the virus. If we suspect that the patients have Covid-19 based on their travel history and respiratory problems, we should use the PPE with gloves, gowns, eye gears, and a special N-95 mask. There is a protocol on how to wear and take off the PPE, as we are at high risk while taking it off. We get special training for that.
What are the procedures the doctors in quarantine need to follow?
If the doctors do not show any symptoms, they do not need to be quarantined. However, those with the virus do not necessarily show symptoms, so it is hard to tell. Therefore, they need to strictly follow the universal assumption of risk approach and PPE protocol while washing their hands regularly and avoiding interactions as much as possible. If they show any symptoms, they must isolate themselves promptly, even from the family members, and get tested for the coronavirus. A few of my colleagues have been at home in isolation.
Of late, there are reports in Nepal like doctors working at ‘coronavirus dedicated’ hospitals got mistreated in society and at homes. Is there any such case there?
Such news from Nepal makes us sad. Thankfully, to date, doctors in Atlanta are getting respect and support from society. Every night, the locals here cheer for us and the hospital administration has also been equally supportive. This is a difficult time for all of us and doctors are working continuously, putting their lives at risk. This is the time when we need support from everyone. Having said that, the doctors should not forget their duty to treat patients of all kinds and follow the protocol while doing it.
Meanwhile, the government has given guidelines to restrict our movement to essential work only, but there is not any lockdown like in Nepal. However, the state is suffering just like Nepal due to the lack of testing samples.
What are the standards to follow to keep an infected person in an ICU?
Each hospital has its own requirements for ICU placement. In general, those who have failing respiratory status, or require IV fluids or other medicines to support their blood pressure should be kept in the ICU. Even in the ICU, these patients must be isolated and the health workers must wear PPE properly while treating them.
Some hospitals have restricted the movement of doctors in and out of the ICUs by having someone deliver the medicines outside the ward and communicating via phone. They have managed iPads for the patients to communicate with their relatives.
There is a stress for contact tracing and testing as a measure to control the spread of the virus here in Nepal. Why is it important?
The patients infected with the virus might not show symptoms until 14 days post-exposure. However, asymptomatic patients can infect others. It has been speculated that on average, one patient can infect two to three people before they begin to have symptoms. Through contact tracing and testing, we can prevent the person from infecting hundreds of thousands of people.
Who is at a higher risk of getting infected among the health workers, ambulance workers, nurses or OPD doctors? How and why?
There are different kinds of PPEs: droplet, contact and airborne. While treating the coronavirus patients, if patients are being intubated or given treatment that includes nebulisation or BiPAP, the providers need to have airborne precautions with an N95 mask. Otherwise, droplet and contact precaution is enough. This includes a surgical mask, eye shield, gloves, and gown. If anyone is suspected of having the virus, the ambulance drivers should also use the PPE like the doctors while transporting them. In case they do not work with the patients, a simple mask is enough.
The coming two weeks can result in an increasing number of cases. For now, we have enough PPE sets for a month, but there is a chance that the virus will still overpower us. The capacity of the state and the hospital is decreasing day by day. We are asking the citizens to follow healthy habits and preventive measures, to prevent the spread of the virus.
There is a lack of PPE sets in Nepal as well. What can be the alternatives of the PPE for doctors to be secure?
Without PPE, it is difficult for providers to be safe. In case there is nothing, the least a doctor will need is an N-95 mask to cover his/her nose and mouth while treating the Covid-19 patients. Without it, they are at high risk of getting infected. But we need full sets of PPE and the health workers need to advocate for that.
Finally, do you have anything to say about the current crisis with a focus on Nepal?
The coronavirus is the biggest challenge of our generation when the health workers are the soldiers. The situation is the same worldwide and no powerful government has been able to control it. If the cases increase in Nepal, the current health system will not be able to cater to it. All the doctors, citizens and the state should understand this and be prepared for it now. To be prepared, the government and administration must focus on PPE and contact tracing and testing, while the public needs to follow public health measures like washing hands, coughing/sneezing properly, social distancing, etc.