The government will not conduct the health insurance programme in private hospitals and medical colleges. But point number 238 of the budget for the fiscal year 2023/24, approved by the House of Representatives on June 13, includes the provision for the implementation of a health insurance programme in government, community, and cooperative hospitals.
According to the budget statement of the current fiscal year, former finance minister Janardan Sharma specified that the implementation of the health insurance programme would be limited to community and government hospitals.
Due to protests regarding favouritism towards private entities, the initial plans to involve insurance companies in the health insurance programme were abandoned. Consequently, the programme was terminated in 14 private hospitals and medical colleges, shifting the focus solely to community and government healthcare facilities.
Now, Finance Minister Prakash Sharan Mahat plans to restructure the health insurance programme, limiting the implementation of the health insurance programme to government, community, and cooperative hospitals. But, officials from the Ministry of Health and Population, along with the Health Insurance Board, express concerns that abruptly closing the programme in private hospitals without a proper restructuring plan in place could have detrimental effects on the health insurance programme.
Need for a better plan
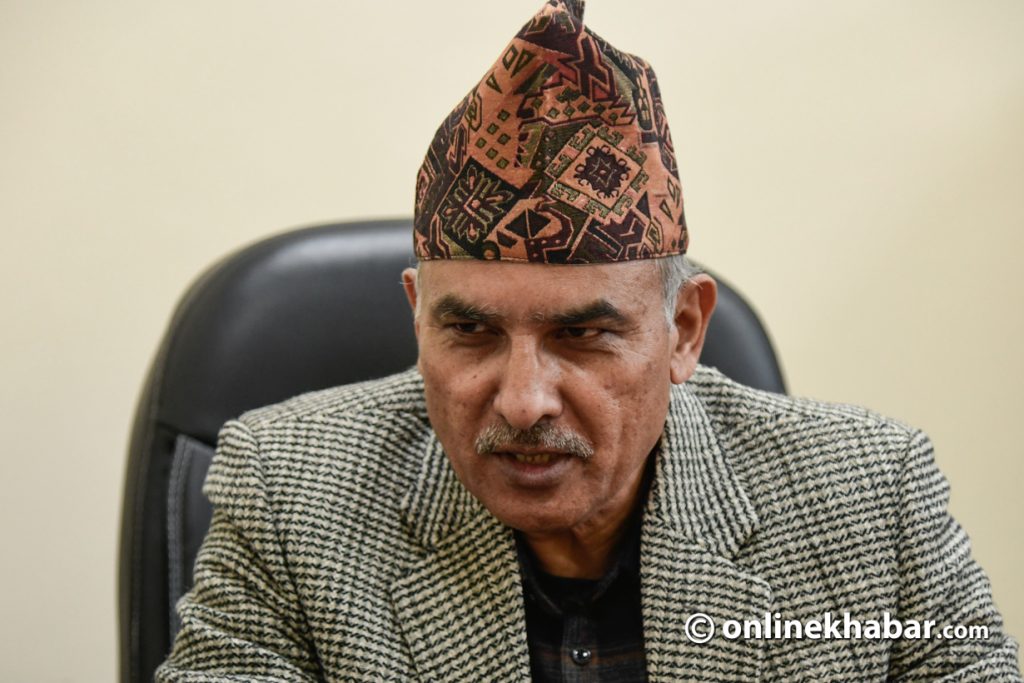
According to the Executive Director of the Insurance Board, Dr Damodar Basaula, the finance ministry did not consult the board before taking the decision to exclude private hospitals and medical colleges from running the health insurance programme. Officials from the health ministry also claim to be unaware of this particular aspect mentioned in the budget statement.
Basaula says operating the health insurance programme with the current model is placing an excessive burden on the government. He suggests that the existing operating model deviates from the fundamental principles of insurance, leading to inefficiencies and challenges in achieving the program’s intended goals.
“Since the insurance cannot increase the coverage, the question arises as to how long the government will be able to bear the burden,” says Basaula.
According to officials from the Ministry of Finance, there are allegations that private hospitals and medical colleges engage in fraudulent billing practices and unnecessary medical tests to take advantage of the benefits offered to insured individuals. As a result, a decision has been made to restrict the provision of insurance services exclusively to government and community hospitals, aiming to address these concerns and ensure the effective utilization of resources.
“Due to rampant abuse in the insurance programme, the provision of services from private and medical colleges has been discontinued,” says Dhani Ram Sharma, spokesperson of the health ministry.
He says that now there is a plan to restructure the health insurance programme for sustainability.
Experts say that the closure of services in private and medical colleges without planning for restructuring has created more problems.
“Government should have identified the weaknesses in the health insurance programme and done something to solve the problem,” health service expert Dr Kiranraj Pandey says. “Instead of solving one problem, the government has brought another big problem. Insurance cannot be sustained without purchasing health services from the private sector.”

The abrupt closure of services in big hospitals
As per the Health Insurance Act-2017, the initial step for obtaining insurance services is to visit a government hospital or health institution. If the required treatment is not available at the government facility, there is a provision to seek services from private hospitals or medical colleges that have been referred and authorised to provide specialised services under the insurance programme.
This approach ensures that individuals receive appropriate care and access to specialized treatments when necessary.
The Act covers privately run hospitals, teaching hospitals along with nursing homes, polyclinics and clinics. According to the data provided by the Insurance Board, there are 464 health institutions listed across the country for health insurance coverage.
Among these institutions, 52 are private health facilities, and their contribution to the insurance program amounts to approximately 30 per cent. This highlights the significant participation of private health institutions in the overall health insurance landscape.
Due to the government’s decision to exclude private hospitals and medical colleges from the health insurance program, private hospitals have withdrawn their participation from the programme.
As a result, the insured citizens have to go to the government hospital, or else they have to be deprived of insurance services. Furthermore, this decision will pose additional challenges to the government’s policy of progressively transitioning the social security programme under the umbrella of health insurance.
Currently, insured individuals continue to face various challenges in accessing timely medicines and healthcare services. They often encounter long waiting times, discrimination between insured and non-insured patients, and the need to purchase medicines from private pharmacies when they are unavailable at hospitals. Moreover, designated health institutions for insurance services in remote areas are often too distant, preventing common people from receiving the intended benefits.
The programme, aimed at facilitating access to healthcare, is experiencing a decline in insurance renewals due to dissatisfaction and inconveniences.
To tackle these issues comprehensively, experts emphasise the necessity of making the entire health sector programme inclusive of insurance, extending coverage to all citizens. However, the progress of the integrated health infrastructure development standards and the initiative to deliver quality health services nationwide within a span of seven years has been halted. Moreover, the decision to exclude private health institutions from providing services further undermines the effectiveness of the health insurance programme.
What’s next?

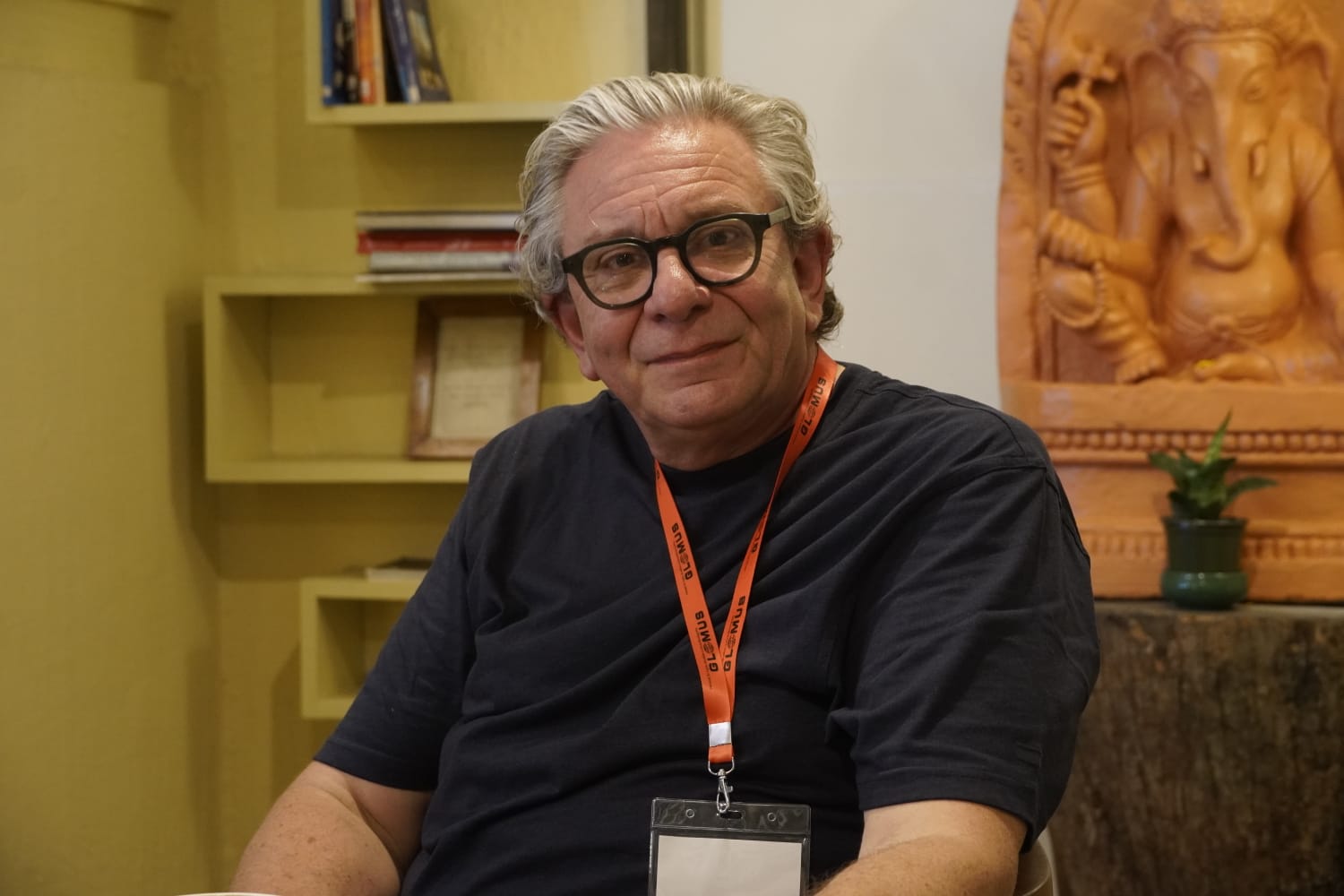
According to Public Health expert Dr Sharad Onta, it is crucial to prioritise services from government-run health institutions. However, he warns that if these institutions cannot ensure satisfactory services and the private sector is also prohibited, the effectiveness of the health insurance programme will be questioned.
Onta emphasises the need for government monitoring and action in case of weaknesses, criticising any reluctance to strengthen the monitoring mechanism or utilise the private sector as a sign of governmental incompetence.
Former Chairman of the Insurance Board, Dr Senendraraj Upreti, disagrees with the complete closure of services from private hospitals. He suggests taking action against organisations engaged in fraudulent practices instead of punishing all private hospitals and medical colleges.
According to the Insurance Board, over 200 private health organisations have applied for contracts. The contracts of four currently serving private hospitals will expire in mid-July. However, the board has halted contract renewals.
Consequently, the number of complaints regarding the lack of services has increased since the health institutions themselves stopped the programme. The Board’s director, Damodar Basaula, states that they have written to the Health, Finance, and Health Committee to seek clarification on the budget statement’s issues.
Basaula further mentions that they are bound by the ministry’s decisions. Health Minister Mohan Bahadur Basnet acknowledges the need for further discussion on the matter and emphasises the government’s responsibility to address the budget’s provisions. He assures that the topic is currently being discussed and coordinated.
This story was translated from the original Nepali version and edited for clarity and length. It is a part of the four-part series.