With the number of active Covid-19 cases crossing 25,000, the government of Nepal looks in a panic. There is a genuine reason behind the panic; the country’s health system has been crippled due to the pandemic. Especially in Kathmandu, intensive care beds have already been scarce for needy patients. The death toll is already increasing, and with the unavailability of essential services, people with other diseases are also likely to suffer more. Apparently, the government has neglected other health problems.
In this context, a team of five Nepali, Indian and Bangladeshi researchers have recently published a report about the impact of the coronavirus outbreak on people living with non-communicable diseases in low and middle-income countries like Nepal. They highlight the pandemic’s impact on such people in under-resourced countries is multiplied by various biological and sociological factors already lying therein, suggesting response strategies should be planned accordingly.
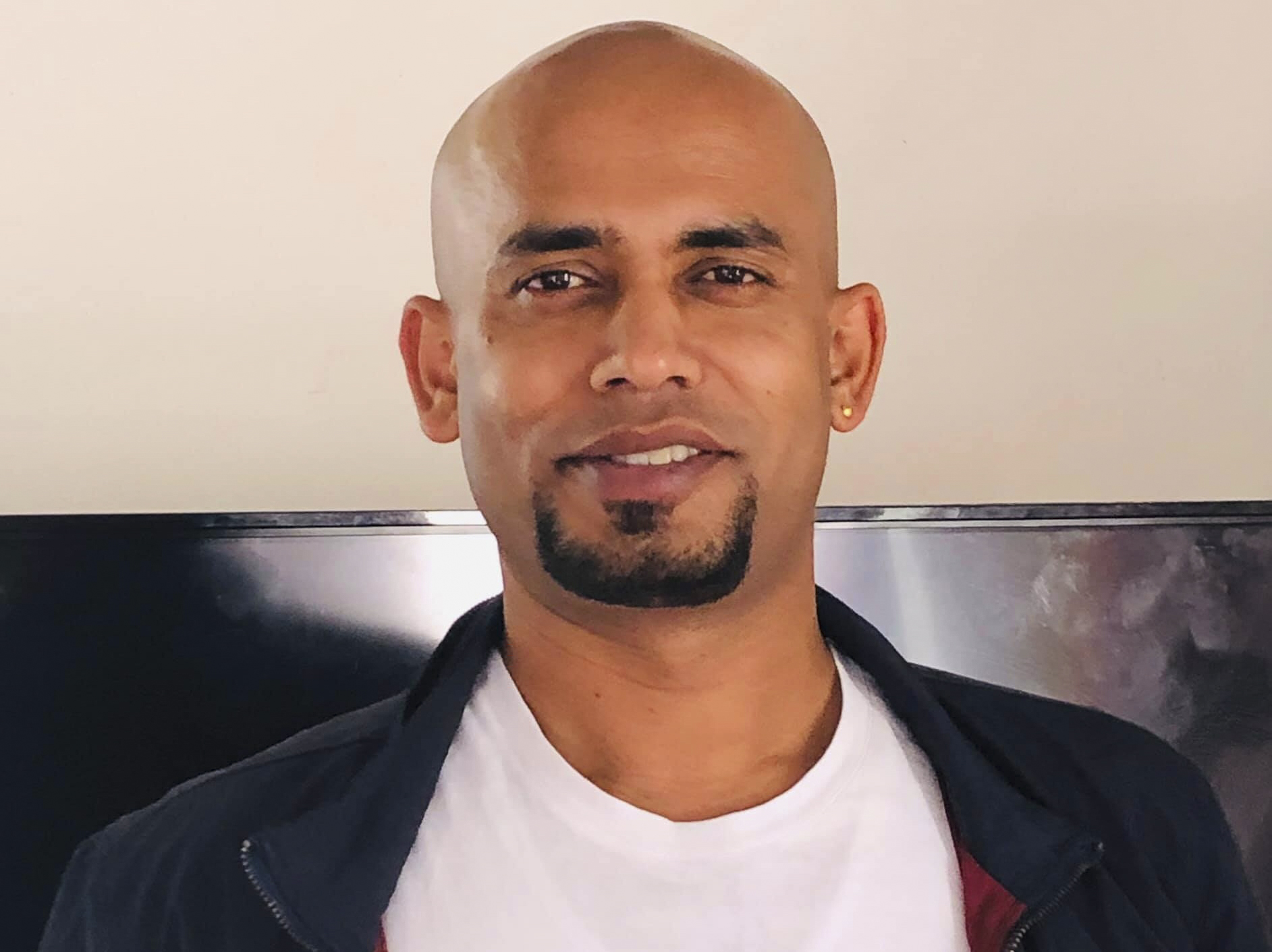
Onlinekhabar has recently talked to Uday Narayan Yadav, the research team’s leader, about the team’s findings and their implication in Nepal.
Excerpts:
Your recent study has concluded that Covid-19 has been a ‘syndemic’ for the people living with non-communicable diseases in low and middle-income countries like Nepal. Can you please explain what it means?
The Covid-19 pandemic has severely impaired the life of human beings from all sectors, but people with non-communicable diseases (NCDs) are suffering from their own diseases more than ever before. Based on an analysis of the evidence, we can see the dangerous face of the pandemic because of its diverse nexus with intertwined biological and socioecological factors. The biological factors include a wide array of NCDs (diabetes, chronic obstructive pulmonary diseases and respiratory illnesses, cardiovascular diseases, cancers, mental health illnesses, frailty, etc) and socioecological factors include social behaviours, physical environment, socio-marginalisation issues and government policies about safeguarding its people.
Such a diverse nexus was called a ‘syndemic’ (synergistic epidemic) by medical anthropologist Merrill Singer in the 1990s to describe the relationship between HIV/AIDS, substance use, and violence. We are reusing this term to describe Covid-19’s interrelation with various biological and socioecological factors this time.
Non-communicable diseases (NCDs) are one of the major public health issues and a leading cause of mortality and morbidity across the world. The NCDs are responsible for more than 71% per cent of global deaths worldwide while the burden is heavier in resource-limited countries like Nepal.
In the same way, the current pandemic has affected all sectors of the population, but the data emerging across the world shows that Covid-19-related complications and mortality are higher among the people living with the NCDs.

How can the impact of the pandemic be different from other people to people with non-communicable diseases?
Currently, government policies and actions have adopted a blanket approach to Covid-19 testing and management. But, we need to base our policies on country-specific data in the time of emergencies. It is not that we should not focus on the general population, but if we can map the high-risk population groups, we can save the lives of vulnerable people like NCD patients.
Data show that the people with the NCDs are more susceptible to Covid-19 and if we see the policies and actions from the government, you cannot see any clear pathways for such people. Instead, people with NCDs are more deprived of health services and care because of nationwide lockdowns and restrictions. Media reports also show that people are not getting admission to hospitals.
Similarly, preventive measures adopted against this pandemic such as physical distancing, self-isolation, and quarantine may increase the exposure to NCD risk factors, such as the increased use of tobacco products and alcohol as coping strategies, increased reliance on unhealthy processed food and barriers to physical activities which lead to negative health outcomes.
The results from a survey conducted by the WHO in 155 countries revealed that people living with the NCDs were not able to access services for their health conditions, which made their lives even more difficult during this crisis. This is supported by the stories and pictures of such people as seen in the news and on social media.
This problem is exacerbated by the reassignment of health staff from NCD facilities to Covid-19 treatment, the disruption of medical supplies and diagnostics, inefficient supplies of essential medicines, and access to health service providers and support service as a result of nationwide lockdowns and similar restrictions.
So, how is it more applicable to low and middle-income countries? Apparently, rich countries also have many people living with non-communicable diseases.
The evidence from low and middle-income countries clearly shows how well health systems and policymakers of these countries are responding to Covid-19 and focusing on priority population groups like people living with the NCDs.
This condition applies to many low and middle-income countries such as Nepal which are crippled with fragile health systems, poor leadership and ineffective implementation of policies. Policies and interventions need to be guided by evidence and experts. Unfortunately, it is not happening, mainly in low and middle-income countries.
That is why, in the current scenario, the term ‘pandemic’ may not be applicable to the low and middle-income countries. Perhaps, a better term would be ‘syndemic’ because a lot of people are dying not because of Covid-19 itself, but because of the syndemic effects of the disease.
The problems you have identified seem obvious. What is tricky is solutions. What solutions do you want to offer for countries like Nepal which do not have enough money and other resources to battle the pandemic?
I do not mean that governments of countries like Nepal are not doing anything. But still, they need to work aggressively in line with the country-specific evidence.
I would not say we lack resources; it is all about priorities for the governments. In any uncertain situation like the current one, the population relies completely on leaders who are in the position to make crucial decisions. But apparently, the Nepali leadership has been entangled in digressive topics: whether or not to accept the Millennium Challenge Corporation grant provided by the US government, whether Lord Ram was born in India or Nepal, whether new vehicles should be purchased for ministers and whether the prime minister needs to be changed. Moreover, the Covid-19 crisis has exposed several other errors that resulted in a scandal in the procurement of Chinese personal protective equipment (PPE) and other medical tools, newly purchased but malfunctioning polymerase chain reaction (PCR) test machines, delays in receiving experts’ opinions for decision making, understaffed and under-resourced public healthcare system, a lack of media management, insufficient supplies and resources, poor planning and inter-sectoral collaboration and support, mismanaged quarantine and isolation centres, and testing processes and a lack of coordination between the three layers of the government system.

Our research report also highlights the need for proper coordination among all levels of governments, public, and private institutions to curb impacts of the Covid-19 pandemic. For example, the government should avoid its attempts to show heroism, instead should listen to experts and stakeholders. It should understand that asking citizens to sacrifice without providing appropriate support packages will not work.
A health literacy campaign and a clear strategy to care for older people and those with existing conditions like the NCDs may also contribute to the effective management of the ongoing pandemic. Involving the private sector, civil society, academia, non-governmental, and governmental organisations through intersectoral coordination and teamwork would address the situation with a syndemic lens. Developmental partners, philanthropists, and industrialists can help Nepal in setting up effective round-the-clock helpline support to provide essential information and guidance related to the availability of services and contact in case of emergency.
The government should take the opportunity to learn from researchers within the country and abroad to address this overwhelming problem.
While the country is struggling to respond to the Covid-19 pandemic in general, do you think it is logical and fair to demand more attention to a particular group of people (for example those with non-communicable diseases)?
Exactly, you got the right point. No one is left behind from the impact of Covid-19. Therefore, to serve the general population and protect it from the pandemic, the government should increase critical care facilities. It should motivate health workers without any political discrimination. Proper care should be provided to those in isolation, including in home isolation.
But, people with the NCDs are at higher risk of dying due to the coronavirus as their immune power is already compromised. Our paper highlights the Nepal government should prioritise the most vulnerable people and give more care to them. We mean to say that effectively managing and treating NCDs patients with cardiovascular and chronic respiratory diseases, hypertension, diabetes and cancer ultimately reduce the mortality of Covid-19 in countries like Nepal. We need to highlight that evidence-guided decisions and interventions are required to overcome this formidable crisis in low and middle-income countries like Nepal.
But, do you think the government of Nepal will respond to such scholarly suggestions like yours?
Our role is to generate and share knowledge and experiences that can help decision-makers to sketch a map for change for its people whom they choose to serve with good science. Nepal has changed a lot in terms of evidence-based practice and I am sure they will take a note of our suggestions to mitigate this overwhelming condition, especially for those who are at a higher risk of Covid-19.
As a Nepali scholar with an insight into the international scenario also, how do you review Nepal’s Covid-19 response? What is Nepal doing right? And, what is going wrong?
I have been observing how leaders in various countries are dealing with the pandemic. I think Nepal can learn a lot from countries like Australia, New Zealand, Singapore, and Vietnam. I would not say that the government of Nepal is way behind in managing Covid-19, but still, there is much to be done, specifically for high-risk and marginalised populations.