
Sandhya Kumari Mahato of Bateshwor rural municipality was fast asleep when a snake slithered into the room and bit the 5-year-old. The young girl was rushed to the community snakebite centre and was later referred to the Phul Kumar Memorial Hospital where she breathed her last.
This is not a solitary case as snakebites in Nepal are a medical emergency. According to a journal, an estimated 40,000 people get bitten by snakes annually and among them, little over 3,000 lose their lives. This is only in the 23 districts in the Tarai and does not include cases that are not reported. And the number is rising every year says Hemant Ojha, head of the Zoonotic Department of Epidemiology and Disease Control Division.
Most of the people who get bit go to the 88 snakebite treatment centre located in 31 districts across Nepal. Apart from that, there are a few government hospitals that treat snakebites too. The Ministry of Health and Population has been purchasing about 2,000 vials of ‘Antisnake Venom’ from India annually and providing it free of cost for snakebite treatment centres and government hospitals.
Despite that, there are a lot of issues as organisations involved are facing a shortage of sufficient anti-snake venom. Additionally, there exists a deficiency in both human resources and infrastructure. The cost of treatment poses a challenge too, particularly for marginalised individuals. Consequently, these individuals are left with the grim choice of either succumbing to the snakebite at home or resorting to seeking treatment from a shaman due to the lack of viable medical options.
Lack of awareness and skilled human resources

According to Krishna Acharya, a senior consultant and anesthesiologist at Bheri Hospital, the time it takes for the venom to disperse within humans varies from 30 minutes to as long as 12 hours, contingent on the specific species of the venomous snake.
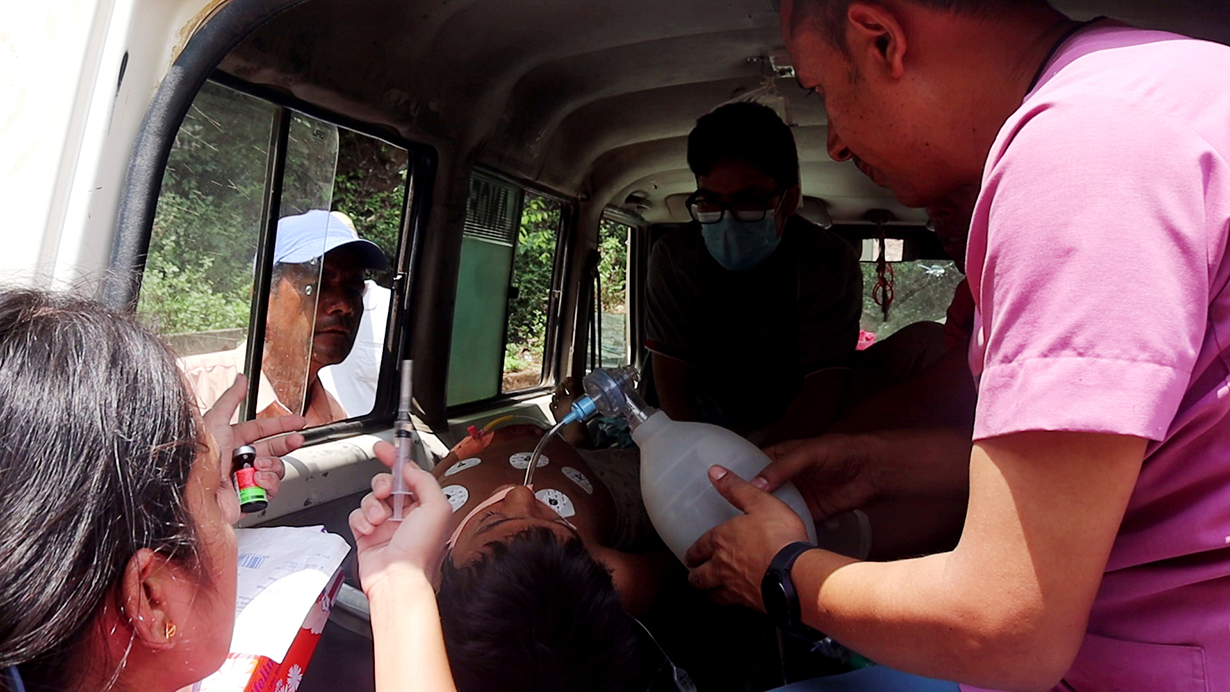
Noteworthy symptoms include stomach ache, vomiting, and respiratory distress. Individuals exhibiting these symptoms should be promptly transported to a medical facility or a specialised snakebite treatment centre for immediate care.
Acharya says that if the patient is taken to the hospital within an hour of being bitten by a snake, there is a 90 per cent chance that the patient can be saved.
But in Nepal, there is a different practice. Most people in rural Nepal go to a shaman instead of a hospital. People only visit a hospital once the situation is critical as a result snakebite deaths are on the rise.
According to the snakebite expert Chhabi Lal Thapa, people are still not well aware of the treatment of snakebites. He informs that in Nawalparasi except for Kali Gandaki Hospital, no private hospital, clinic or college provides treatment for snakebites.
Due to the lack of treatment facilities for snakebites in district hospitals, patients of Pyuthan, Dang, Bardiya, and Kailali have to go to Bheri Hospital, travelling for hours. As time is critical when one gets bitten by a snake, they die as they do not get adequate care on time.
A similar incident occurred in Pyuthan on June 20. Abhishek Nepali was swiftly taken to Bijurwa District Hospital merely ten minutes after being bitten by a snake. The hospital had both a doctor and a supply of anti-snake venom. Regrettably, the doctor on duty lacked the expertise to administer proper treatment for a snakebite victim.
Consequently, the doctor advised Nepali to seek assistance at the district hospital in Dang. But Nepali’s condition deteriorated during the journey, resulting in his death due to the rapid dissemination of the venom throughout his body. Had a proficient doctor been available at the initial hospital, Nepali’s life might have been saved.
Expensive treatment and poverty
Although the government provides anti-snake venom for free, the cost of medicine, oxygen, ICU, ventilator and dialysis needs to be paid by the patient.
“It cost over Rs 100,000 for the treatment of snakebite,” says Acharya.
He further says that Nepal’s policymakers are unaware that snakebite is a health issue for the poor.
“The government has remained indifferent about the pain and suffering that the poor people have to go through due to the snakebite.”
According to Acharya, snakebite is a huge health problem in the country but the ministry, political parties and media have not given it much attention.
The statistics of the Ministry of Health and Population show that in the fiscal year 2021/22, 926 patients with snakebites reached the hospital for treatment spending around Rs 100,000 on average. This is a huge amount for a family who even struggles to fulfil their basic needs.
Hemlal Acharya from Dullu, Dailekh, who travelled to Nepalgunj to seek medical care for his son following a snakebite, said, “In situations where medical resources are not readily available and individuals have to bear the expenses themselves, the treatment costs can range from Rs 500,000 to Rs 700,000.”
Madhav Acharya, a resident of Dullu in Dailekh, had to spend a night at his relative’s residence during his journey to India for employment. There he was bitten by a Krait snake while sleeping there. He underwent a 17-day treatment period at both Kohalpur Medical College and Bheri Hospital.
His condition was critical, leading to a seven-day stay in the intensive care unit (ICU) and another 10 days on a ventilator. Despite the fact that the expenses for the hospital bed and medications were covered by Bheri Hospital, Madhav incurred a total treatment cost of Rs 250,000.
Inadequate government effort and the absence of health insurance

According to public health expert Jeevan Chettri, the government’s focus on the health sector is notably lacking. In such circumstances, matters concerning snakebites are unlikely to receive any form of priority or attention.
Chettri says that poor people who are at risk of snakebites have to go through a lot of economic difficulties. They are unable to put forward their problems to policymakers. Due to this, policymakers are not sensitive to the financial problems caused by snakebites.
But Ojha, who is also a focal person of the Ministry of Health and Population contradicts Chettri says that the government has been providing free anti-snake venom and training to health workers. Likewise, it is also conducting a public awareness programme in collaboration with the Red Cross Society and Rotary Club.
“The government is doing various things to address the problem of snakebite,” says Ojha. “They might be inadequate but it is wrong to say that the government does not care about the snakebite issue.”
However, Chettri says although the government defends itself, even today, poor citizens who have been bitten by snakes are forced to go to a shaman instead of going to the hospital. This condition needs to be studied specifically.
Chettri further says that if the government manages a free treatment of snakebites, the number of people losing their life by going to shamans will decrease.
“In areas with a high risk of snakebites, the government can assist by offering free insurance to the residents,” says Chettri, “Individuals with health insurance should receive free treatment for snakebites. If the insurance covers all the expenses, the death due to snakebites will decrease and the financial burden of the family members will also be reduced.”
Menuka Shahi, nursing officer and focal person of Bheri Hospital says that most of the expenses, including medicine, bed charge and ventilator, of snakebite patients are covered by the health insurance. But the majority of snakebite patients do not have health insurance. Due to the absence of health insurance, they go through a lot to manage fees for the treatment.
Experts say that there is a dearth of awareness about snakebite in a place where there is a high risk of it.
According to experts, menstruating and pregnant women are more prone to snakebites. Because of the belief that menstruating women should not sleep indoors or on a bed, they are compelled to sleep outside in places like the yard, cattle shed, and even makeshift huts. This harmful practice exposes women to an increased risk of snakebites.
In the second week, 15-year-old Hemanti Joshi of Sukhad, Kailali was menstruating and sleeping on the veranda. She was taken to Seti Hospital where she breathed her last.
Another pressing issue is the delayed availability of ambulances for patients. Even when ambulances are accessible, individuals often lack information about the hospitals equipped to provide snakebite treatment. This lack of awareness further complicates the situation.
A study conducted in 2019 and 2020 by BP Koirala Institute of Health Sciences and experts has shown that 40 per cent of deaths due to snakebites occur in villages. The other 40 per cent die on the way and around 20 per cent die amid the treatment.
Small steps

In 2014, Jhalnath Khanal Institute of Health Sciences was formed to produce anti-snake venom (ASV) in Nepal. Under the initiative of former prime minister Jhalnath Khanal, the foundation also received a grant of around Rs 190 million from the federal government and the Madhesh province government.
After receiving the grant money, the foundation purchased about 6.25 acres of land in Lalbandi municipality-1 by spending Rs 700 million. In 2020 the government allotted Rs 720 million for the foundation but due to the change in the government, they did not receive the grant. The government’s decision to provide the grant for the foundation even received flak from netizens.
To overcome the criticism and risk of not getting grants from international donors, the foundation was changed to the National Health Science and Research Council.
“The construction of a farmhouse for snake breeding, a laboratory, a one-hundred-bed capacity hospital and an administration building has been stopped due to the suspension of grants for two years,” says Revati Pant, president of the foundation.
In point number 71 of the budget statement announced by the Madhesh province government on June 16, it is mentioned that the budget will be arranged in a phased manner for the construction of necessary infrastructure after studying the feasibility of anti-snake venom production.
According to Ojha of the Epidemiology and Disease Control Division, Nepal imports 20,000 vials of antisnake venom annually and is sent to snakebite treatment centres and hospitals across the country.
“The anti-snake venom imported from India for treating snakebite patients is not as effective as it is in India,” says Sanjeev Kumar Shah, snakebite expert and acting vice-chancellor at BP Koirala Institute of Health Sciences. “Anti-snake venom made from raw material extracted from snakes found in India can pose a risk of reaction when given to patients bitten by snakes in Nepal.”
He adds that it would be great if anti-snake venom could be produced in Nepal.
Zoologist Kamal Devkota says that except for providing anti-snake venom and three-day-long training to the health workers, the government has not done anything more.
According to Devkota, alongside the government, the donor agencies have also not prioritised the problem of snakebite. He questions, “Why is this problem, not a priority for both the government and donor agencies?”
This story was translated from the original Nepali version and edited for clarity and length.




















